NCLEX Atrial Septal Defect
NCLEX Atrial Septal Defect
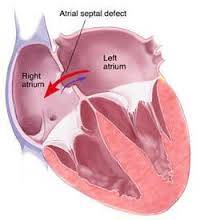
Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria (upper chambers) of the heart. Normally, the atria are separated by a dividing wall, the interatrial septum. If this septum is defective or absent, then oxygen-rich blood can flow directly from the left side of the heart to mix with the oxygen-poor blood in the right side of the heart, or vice versa. This can lead to lower-than-normal oxygen levels in the arterial blood that supplies the brain, organs, and tissues. However, an ASD may not produce noticeable signs or symptoms, especially if the defect is small.
A “shunt” is the presence of a net flow of blood through the defect, either from left to right or right to left. The amount of shunting present, if any, determines the hemodynamic significance of the ASD. A “right-to-left-shunt” typically poses the more dangerous scenario.
Signs and Symptoms
Atrial septal defect signs and symptoms may include:
- Shortness of breath, especially when exercising
- Fatigue
- Swelling of legs, feet or abdomen
- Heart palpitations or skipped beats
- Frequent lung infections
- Stroke
- Heart murmur, a whooshing sound that can be heard through a stethoscope
Causes
An atrial septal defect (ASD) allows freshly oxygenated blood to flow from the left upper chamber of the heart (left atrium) into the right upper chamber of the heart (right atrium). There, it mixes with deoxygenated blood and is pumped to the lungs, even though it’s already refreshed with oxygen.
Atrial septal defects can be several types, including:
- Secundum. This is the most common type of ASD, and occurs in the middle of the wall between the atria (atrial septum).
- Primum. This defect occurs in the lower part of the atrial septum, and may occur with other congenital heart problems.
- Sinus venosus. This rare defect occurs in the upper part of the atrial septum.
- Coronary sinus. In this rare defect, part of the wall between the coronary sinus — which is part of the vein system of the heart — and the left atrium is missing.
Risk Factors
It’s not known why atrial septal defects occur, but congenital heart defects appear to run in families and sometimes occur with other genetic problems, such as Down syndrome. If you have a heart defect, or you have a child with a heart defect, a genetic counselor can estimate the odds that any future children will have one.
- Rubella infection. Becoming infected with rubella (German measles) during the first few months of your pregnancy can increase the risk of fetal heart defects.
- Drug, tobacco or alcohol use, or exposure to certain substances. Use of certain medications, tobacco, alcohol or drugs, such as cocaine, during pregnancy can harm the developing fetus.
- Diabetes or lupus. If you have diabetes or lupus, you may be more likely to have a baby with a heart defect.
- Obesity. Being extremely overweight (obese) may play a role in increasing the risk of having a baby with a birth defect.
- Phenylketonuria (PKU). If you have PKU and aren’t following your PKU meal plan, you may be more likely to have a baby with a heart defect.
Complications
A small atrial septal defect may never cause any problems. Small atrial septal defects often close during infancy.
Larger defects can cause mild to life-threatening problems, including:
- Right-sided heart failure
- Heart rhythm abnormalities (arrhythmias)
- Increased risk of a stroke
- Pulmonary hypertension. If a large atrial septal defect goes untreated, increased blood flow to your lungs increases the blood pressure in the lung arteries (pulmonary hypertension).
- Eisenmenger syndrome. In rare cases, pulmonary hypertension can cause permanent lung damage. This complication, called Eisenmenger syndrome, usually develops over many years and occurs only in a small percentage of people with large atrial septal defects.
Treatments
Many atrial septal defects close on their own during childhood. For those that don’t close, some small atrial septal defects don’t cause any problems and may not require any treatment. But many persistent atrial septal defects eventually require surgery to be corrected. Once someone is found to have an atrial septal defect, a determination of whether it should be corrected has to be made. Methods of closure of an ASD include surgical closure and percutaneous closure.
Surgical mortality due to closure of an ASD is lowest when the procedure is performed prior to the development of significant pulmonary hypertension. The lowest mortality rates are achieved in individuals with a pulmonary artery systolic pressure of less than 40 mm Hg.
NCLEX National Exam Courses
Overview
- Elite Reviews Offers A Variety Of Online Courses That Will More Than Adequately Help Prepare The Graduate Nurse To Pass The National Exam.
- Each Course Includes Sample Questions & The Most Current NCLEX Exam Updates.
NCLEX Free Trial
- FREE Sample Lecture & Practice Questions
- Available For 24 Hrs After Registration
- Click The Free Trial Link To Get Started – NCLEX Free Trial
How It Works
How The Course Works
- First – Purchase The Course By Clicking On The Blue Add To Cart Button – You Will Then Be Prompted To Create A User Account.
- Second – After Creating An Account, All 3 Options (90, 120, 150 Days) Will Be Listed. Select The Option You Desire And Delete The Other Two.
- Third – You Will Be Prompted To Pay For This Review Using PayPal – After Payment You Will Be Redirected Back To Your Account.
- Last – Click The Start Button Located Within Your Account To Begin The Course
- 175 Prep Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $75.00
- 1250+ Prep Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $200.00
NCLEX Practice Questions Bundle
- 1350+ Prep Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $225.00
NCLEX Review Course
- Option 1
- Lectures & 1250+ Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $275.00
- Option 2
- Lectures & 2000+ Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $325.00
NCLEX Review Course Bundle
- Option 3
- Lectures & 3000+ Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $375.00